Coma R40.20, Is this appropriate for final coding and reporting without TBI?
Recently during audit and collaboration with my team of Coding Professionals regarding a finding of missed documentation r/t Dx Coma POA R4020 with identified impact to SOI, ROM, and expected mortality. The coding professional did not support finding with rationale:
The coma scale codes (R40.2-, Coma) can only be used in combination with traumatic brain injury codes, thus, not appropriate for this encounter. This is a coding guideline not a clinical guideline. As such, this guidance isn’t meant for clinical dx of a patient, rather, how to report the ICD-10-CM codes.
Based on the update to the coding guidelines on October 1, 2020 my understanding is a limitation of the GCS/Coma scale codes requiring a TBI for accurate final coding and reporting and not R4020 Coma, unspecified.
I'm curious how other facilities capture and report R4020 Coma, unspecified with the current perspective set with our department that it is only reportable with TBI. I really want to dive into the accurate capture and reporting of Coma on those cases that do not have a TBI....clinically I am having a hard time accepting that we are unable to accurately report the pts SOI and ROM to include Coma for those cases without TBI. In addition, a need for clarification and understanding to assure we are doing the right thing and accurately reporting the resource consumption, true clinical picture of patients SOI/ROM, hard work, and quality care provided.
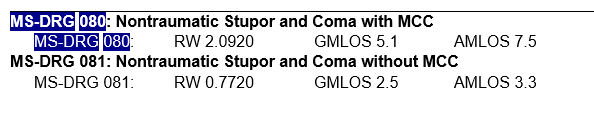
In my research findings also surfaced a DRG for Non-traumatic w/Coma...this would contradict the guideline if it is meant to encompass R4020....
Thoughts, please? Thanks for your feedback, support, guidance, and time :)



Comments
F/U: our team submitted a question to Nosology and FY2022 changes to ICD-10 and IPPS assisted in clarification regarding Coma capture and reporting. Long story short, yes, Coma R4020 is a sign/symptom code, it is not integral to most disease processes and therefore should be captured when documented.
Nosology Question sent:
Can R4020 coma unspecified be coded with other condition; such as; strokes, heart conditions, seizure, etc; or can they only be used with TBI?
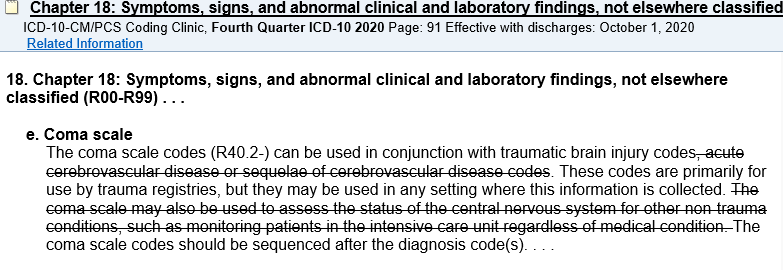
e. Coma scale
The coma scale codes (R40.2-) can be used in conjunction with traumatic brain injury codes. These codes are primarily for use by trauma registries, but they may be used in any setting where this information is collected. The coma scale codes should be sequenced after the diagnosis code(s). . . .
Continued collaboration r/t specification/terminology of the Coma Scale codes (R40.2-) as those primarily for use by trauma registries and should only be reported with TBI as a subcategory of R40.20. Coma, unspecified (R40.20) is not included as a code used for trauma registries for GCS specification and would not be an inclusion to the coding guideline for final coding and are reporting.
Nosology Response received:
It is appropriate to report code R40.20 Unspecified coma, from the sign or symptom section as additional diagnosis for the documentation "coma" or "comatose" that is not integral to another condition such as stroke, heart conditions, seizure, TBIs or other conditions.
I would not report both R40.20 (unspecified coma) AND coma scale codes when the coma scale values are reported in the medical record.
The Official Guidelines for Coding, Section I.C.18.e. that you referenced is addressing Coma Scale; which can be used in conjunction with traumatic brain injury codes. Coma scale codes are R40.21- range, while the coma diagnosis is code R40.20.
The 3m Clinical Documentation Improvement System Reference states how Coma is an important severity and mortality driver. While coma is a sign/symptom code, it is not integral to most disease processes and therefore should be captured when documented.
AHA Coding Clinic® for ICD-10-CM and ICD-10-PCS,Second Quarter 2015, pages 17-18 and Fourth Quarter 2016, pages 64-65
FY2022 changes to ICD-10 and IPPS:
Chapter 18: Symptoms, signs an abnormal findings (R00-R99), 1) Coma Scale, Code R40.20, Unspecified coma, may be assigned in conjunction with codes for any medical condition.
Just wanted to share and close the loop in case others find themselves with this question/need for clarification😁
Beating a dead horse...
R40.20 but recognize that this code can be coded for stroke. but "wouldn't code both"...
I know many ( not all) institutions are only coding GCS and individual components with TBI...
I do not understand this since a "1" in GCS is excluded as an MCC and shows X in encoder. BUT it registers as an MCC if coded with a CVA.
I get many people interpreted "may code" to mean "can ONLY CODE"
but, if GCS can only be coded with TBI, why would it ever show up as an MCC for anything- WHY NOT JUST REMOVE IT FROM THE MCC LIST?
i appreciate any input or instance when the components would be MCCs?
Thank you!
Ann
2022
Coma Code R40.20, Unspecified coma, may be assigned in conjunction with codes for any medical condition.
Do not report codes for unspecified coma, individual or total Glasgow coma scale scores for a patient with a medically induced coma or a sedated patient. 1) Coma Scale
The coma scale codes (R40.21- to R40.24-) can be used in conjunction with traumatic brain injury codes. These codes are primarily for use by trauma registries, but they may be used in any setting where this information is collected. The coma scale codes should be sequenced after the diagnosis code(s). These codes, one from each subcategory, are needed to complete the scale. The 7th character indicates when the scale was recorded. The 7th character should match for all three codes. At a minimum, report the initial score documented on presentation at your facility. This may be a score from the emergency medicine technician (EMT) or in the emergency department. If desired, a facility may choose to capture multiple coma scale scores.
ICD-10-CM Official Guidelines for Coding andReporting FY 2022 Page 72 of 115 Assign code R40.24-, Glasgow coma scale, total score, when only the total score is documented in the medical record and not the individual score(s). If multiple coma scores are captured within the first 24 hours after hospital admission, assign only the code for the score at the time of admission. ICD-10-CM does not classify coma scores that are reported after admission but less than 24 hours later. See Section I.B.14 for coma scale documentation by clinicians other than patient's provider