Best Practice Advisory Use in OP CDI Programs.
Hello - If you use EPIC, can you please share your workflow for using BPA's for suspected conditions? Does you/your CDI populate the pre-visit documentation form with the diagnosis and ICD-10 code so it can be accepted or rejected by the provider? Has compliance weighed in? At the ACDIS conference there was a WIDE range of opinions of 'no way' to 'it's okay.'
Thank you.
Alison
Alison.White@cvmc.org
Tagged:


Comments
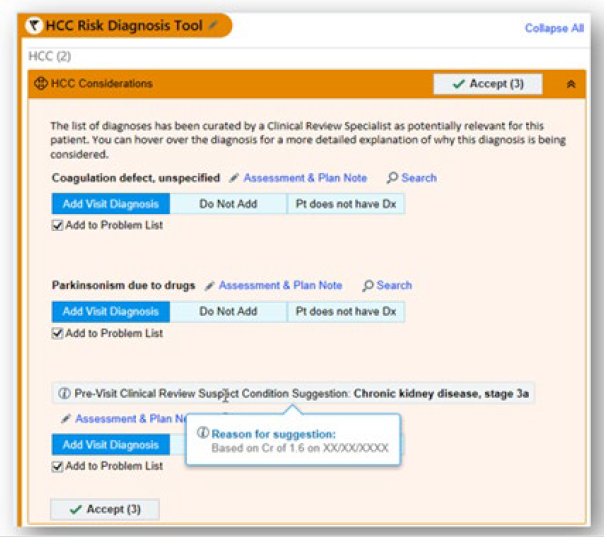
Thank you for sharing your image. We are just starting to build an OP CDI program, and with or last Epic upgrade some of these features have just become available.
I am sure I will have more to add as we start exploring these options. I hope you don't mind, but I would like to connect with you to get some of your thoughts and experiences.
Best regards,
Tamara
Tamara.Breyer@uchealth.org
Please feel free to reach out.
We are currently utilizing a BPA in EPIC for HCC capture. We have a smartform which is divided into 3 sections, Suggested, Add and N/At patient/Resolve. CDI places suspected diagnosis from outside sources along with clinical evidence to support diagnosis in the suspected section - they do not comment on whether to add /resolve the diagnosis. The Add and Resolve sections are for HCC recapture from our healthsystem. For recapture, our CDI is able to suggest to resolve or add along with clinical data to support their decision. There is a note section at the bottom in which the CDI is able to add guidelines related to the diagnosis. This did pass our compliance department. We are currently asking compliance for our CDI to be able to add diagnosis they suggest to the BPA....we are just at the beginning of that process.
Our Ambulatory CDI program is very new and I'd appreciate any tips your Ambulatory CDI program has found.
-Jenny
Jenny.Peters@Bellin.org
I'm so glad I stumbled onto this conversation. Our outpatient CDI program just started using Optum Clinivations. It is very similar to the Epic BPA. The providers can use the HCC Smartform to address the condition or indicate it doesn't apply or is resolved. Mixed results so far. I worry that a cancer diagnoses needs more documentation than "Under treatment or active surveillance by appropriate specialist". Providers can choose this statement on the HCC Form. If they are on treatment, I really like for that to be documented, including what medication.
Any thoughts?
Thank you,
Sarah
slaconis@bch.org
Hi all,
I need to resurrect this thread to learn from you all.
Our OP CDI program has worked mostly in Athena & we are now expanding into our first Epic network. I have sent prospective queries via Epic before but have never used the BPA (now OPA) functionality. I find this to be clunky for our needs, so hopefully I'm missing something. @https://forums.acdis.org/profile/jenny.peters%40bellin.org I really appreciate your explanation of the smartform functionality, can you direct me to a resource to provide further clarity?
My other questions center around how to pull back information out of Epic to understand how providers are interacting with OPAs.